HIP REPLACEMENT SURGERY MELBOURNE
Hip Replacement Surgery Melbourne – A patient’s guide
Dr Arash Riazi – MBBS, BSc (Med), FRACS (Ortho), F.A.Orth.A.
Orthopaedic Surgeon.
 This guide is to help you understand the benefits and limitations of total hip replacement surgery.
This guide is to help you understand the benefits and limitations of total hip replacement surgery.
It explains what hip replacement surgery is, who could benefit, what to expect, potential complications and recovery information that may help you get the best results from your surgery.
If you have any questions about total hip replacement surgery, please contact my offices using the details below.”
Dr Arash Riazi – Orthopaedic Surgeon
If you have any questions please call
(03) 9898 4216
New patients welcome.
Please bring a referral from your GP or Specialist.
Learn more about hip replacement surgery
Access the buttons below to be taken directly to the relevant information:
What is hip replacement surgery
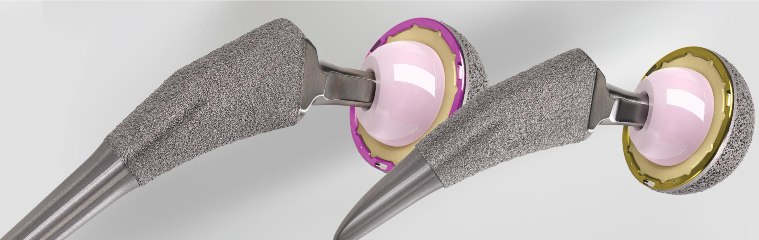
Total hip replacement surgery (also called total hip arthroplasty) involves removing the damaged bone and cartilage in your hip joint and replacing it with an artificial joint, made of highly durable metal and plastic components.
Hip joints are composed of two parts; the hip socket (acetabulum) and a ball (femur). A total hip replacement involves removing these two parts and replacing them with an artificial joint.
Dr Riazi is trained in both anterior and posterior approaches to hip replacements. Depending on your anatomy one method may be safer and more suitable than the other. Both techniques are minimally invasive and both approaches may allow you to be up walking the day after your surgery.
Why consider hip replacement surgery
If your hip has been damaged by arthritis, a fracture, or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult.
When all other treatment options have failed to provide adequate pain relief such as medications, changes in your everyday activities, and the use of walking supports, you may consider hip replacement surgery. The procedure aims to relieve a painful hip joint, making walking and other everyday activities easier.
Hip replacement surgery is considered a safe and effective procedure that may relieve your pain, increase motion, and may help you get back to enjoying normal, everyday activities.
During total hip replacement surgery
An anaesthetist will assess you and decide on the most suitable form of anaesthetic. Usually you are given a general anaesthetic so that you are completely asleep during the operation.
Dr Riazi will see you before the operation to answer any questions you may have and mark the site of surgery.
During the procedure an incision will be made and the part of your hip that is being replaced will be cut out and replaced with a prosthesis.
The procedure usually takes about 2 hours.
Hip Replacement Surgery Melbourne
Types of hip replacement surgery
1. Anterior Hip Replacement
The anterior hip replacement approach is from the front of the hip joint as opposed to a lateral (side) approach to the hip or posterior (back) approach. One of the big advantages of the anterior approach is that the most important muscles for hip function, the gluteal muscles that attach to the posterior and lateral pelvis and femur, are left undisturbed.
Other surgical approaches may need to detach multiple muscles from the femur during surgery. In the anterior approach, the hip is approached and replaced through a natural interval between muscles resulting in less trauma and recovery time.
Dr Riazi is certified to perform minimally invasive anterior hip replacement procedure and has successfully completed all the necessary training required to undertake anterior hip replacement.
Advantages of this approach:
- Less damage to major muscles in the hip – There are fewer muscles at the front of the hip
- Less post-operative pain – Anterior approach does not require cutting major muscles
- Faster recovery – Most patients can bend at the hip and weight bear weight soon after surgery
- Wound positioning – Patients can lie on their back during the recovery process
- Realtime imaging – This allows for an accurate positioning of the artificial hip components
- Decreased risk of hip dislocation – Anterior hip replacement surgery does not disturb the muscles and soft tissue structures that naturally prevent the hip from dislocating
- Studies reveal – Anterior approach is slightly quicker to recover in the first few weeks, however by 6 weeks both Anterior and Posterior approaches are functionally the same.
Disadvantages of this approach:
- Suitability – Not suitable for all people due to anatomical differences.
- Fracture risk – Slightly higher risk of fractures due to difficulty in seeing the femur in certain patients
- Bleeding – Slightly higher risk of bleeding
- Thigh pain or numbness – Reported cases of thigh pain or numbness due to the lateral cutaneous nerve of the thigh injury or scar tissue in the tensor fascia lata.
2. Posterior hip replacement
This approach is very extensile and useful in both primary and revision hip replacement. It is the most commonly used approach by Dr Riazi. It can be done through a minimally invasive technique, however it does involve cutting small tendons at the back of the hip which require formal repair.
It is done through a small cut on the side of the hip. The hip is dislocated through the back of the hip capsule and hence special precautions need to be taken in the first 6 weeks until these structures heal. Often no X-ray or image intensifier is required as the patient’s own anatomy is used for landmarks. In certain cases computers are used to navigate positioning of the components.
Advantages of posterior hip replacement:
- High success rate – Very common procedure
- Minimally invasive – Minimal muscle damage
- Accuracy – More precise placement of implants and excellent visibility of the joint
- Small incisions – Pleasing cosmetic results
- No difference in function to Anterior approach at 6 weeks post-operatively.
Disadvantages of posterior hip replacement:
- Potential for nerve injury – Slight risk to sciatic nerve injury (less than 1%)
- Hip dislocation risk – Theoretical risk of dislocation due to weakness in the posterior structures (less than 1% risk)
- Recovery – Slightly longer recovery in the first 6 weeks.
3. Anterolateral (Modified Hardinge Approach)
Dr Riazi uses this approach in cases where there is severe hip stiffness (fixed flexion deformity) as it allows releasing of certain deforming structures. It also allows repair of gluteal tendons if they are torn and to remove bursal tissue.
This approach is also done with the patient on their side and through the gluteal tendons which later would be formally repaired.
It is traditionally used for fractures however its use is declining due to the weakness it causes the gluteal muscles and the subsequent limp which can last for up-to a year.
Advantages:
- Ideal for patients with severely stiff hips
- Gluteal repair – It allows repair of gluteal tendons
- Stability – It is extremely stable
- Visual – Allows excellent visual access for the surgeon of both the acetabulum and femur
- Can be extensile and used in revision surgery
Disadvantages:
- Limp – Patients may walk with a limp for up to 12 months after the surgery
- Slower recovery – Longer recovery times are associated with this surgery.
Preparing for hip surgery with Dr Riazi
Once the decision is made between yourself and Dr Riazi to have surgery, his team will help prepare you for the operation. Here is a checklist to help you prepare:
1. Medical Conditions
Please ensure you notify Dr Riazi about any medical conditions you have. We also recommend you make an appointment with your GP to assess:
- Your general health prior to your surgery
- Your fitness for surgery and anaesthesia
- The need for pre-operative tests such as blood tests, cardiogram and/or a chest x-ray.
If you have any dental work planned, make sure that it is completed well in advance of surgery. It is important that any dental infections are dealt with prior to joint surgery, due to the potential risk of infection.
In the week before surgery if you experience any cold symptoms, fever or other illness, please notify Dr Riazi immediately.
2. Medication
If you are taking any medication, including herbal medicines please let Dr Riazi know. Please bring in a list of your medications to your appointment with Dr Riazi and when you come into hospital for surgery.
Medicines that thin your blood will need to be stopped before surgery. Also some other types of medication such as corticosteroids and insulin will also need to be managed before and after surgery. If you have any questions about your medicines please contact Dr Riazi.
3. Smoking
Smoking increases your risks of problems during and after surgery, including risk of infection. Stopping smoking before your procedure and staying smoke free during recovery may substantially improve wound healing as well as your general health. We advise you contact your GP to help you develop a plan to quit smoking before your surgery.
4. Keeping fit
It is important to try and be as fit as possible before surgery to reduce the chance of complications and reduce the length of your recovery. Your GP will be able to provide you with further advice.
5. Fasting guidelines
Dr Riazi will advise you regarding the fasting recommendations. In general, for morning surgery we advise to fast from midnight the night before the procedure and for surgery scheduled for the afternoon patients should fast for 6 hours prior to admission on the day of surgery. You can have clear fluids up until 2 hours before surgery.
6. Home Preparation
There are a number of measures you can take to prepare for coming home after surgery.
- Rearrange the furniture so that you can easily manoeuvre throughout your home
- Remove any rugs or throws that may cause a fall
- You may need to install special equipment for use in your bathroom such as a shower chair, handrails or a raised toilet seat.
Other items that can be useful are long handled shoehorns and grabbing tools or reacher. Place items that you need to use such as mobile phone, remote control and medicines near where you sit.
You may also need assistance with household chores like cooking and shopping, so plan ahead for this. It is a good idea to prepare and freeze some meals ahead or arrange for someone to bring meals to you.
Hip replacement surgery Melbourne
Possible complications
Bleeding – There is a risk of blood loss during the procedure and sometimes a blood transfusion may be required.
Venous Thromboembolism (VTE) – A VTE is when there is a blood clot inside a blood vessel. There are two types of VTE:
- Deep Vein Thrombosis (DVT) – this is a blood clot that forms in a vein, usually in the leg. Signs and symptoms include redness, swelling and pain but sometimes there are no symptoms at all.
- Pulmonary Embolism (PE) – is when the blood clot becomes dislodged and travels to the lung. Symptoms of a PE include chest pain, breathlessness and coughing.
All patients are given measures to prevent a VTE from happening. These may include blood thinning medications and below the knee compression stockings. It is important to move around as soon as possible after surgery. The nursing and physiotherapy staff will help you.
Infection – There is a risk of infection in the wound site. You will be given antibiotics both during and after your surgery to help prevent this. If an infection does still occur, you will be given antibiotics to help clear it up.
Pain – With any surgical procedure, you may experience some pain. Dr Riazi and the medial staff use various anaesthetic techniques to minimise this and provide you with painkillers to help manage your pain. It is important that you get adequate pain relief so that you are able to move around as soon as possible after your operation.
Anaesthesia risks – Your anaesthetist will meet with you before the operation and discuss the risks with you as well as the best option for you.
Dislocation of the hip – There is a very small risk of dislocation of the hip. This is when the ball pops out of the socket. It could happen at any stage however the highest risk is the few days and weeks following surgery. A physiotherapist will see you after surgery. It is important to follow their advice on strengthening exercises and general movement to prevent this from happening.
Please contact hospital staff or Dr Riazi immediately if:
(1) Your hip or calf becomes more swollen, red and/or hotter or more painful than before
(2) Fever or night sweats
(3) Clicking or sensation of instability in your hip joint
(4) A “popping” sounds of the hip
After your operation
After your operation you will be transferred to a hospital recovery room where you will be closely monitored and then to a surgical ward where nursing staff will look after you. We aim to have you out of bed and moving and using your new hip as soon as possible after the operation. This may help speed your recovery and reduce the chances of a blood clot.
Physiotherapy
A physiotherapist will help get you moving around as early as day 1. They will be there to guide you and show you strengthening exercises to make your muscles stronger and show you the movements you need to avoid.
Post surgical follow-up
On the day after your surgery Dr Riazi and a specialist physician will see you. You will have been given pain medication to help manage any aches or discomfort as effectively as possible, so that you are able move around.
We aim to send most patients home by day 3 although some patients may take longer to recover. You may need to use crutches in order to walk for 3-6 weeks. By following your physiotherapy program effectively you may be able to walk around without crutches sooner.
IMPORTANT NOTE
This information is designed to be a guide only. Every patient has unique needs and will react differently to surgery, pain management and recovery approaches.
If you would like more details or have any worries or questions about hip replacement surgery please contact my offices so I may address your concerns.
HIP REPLACEMENT SURGERY MELBOURNE
Dr Riazi consults with private and public orthopaedic patients from all over Melbourne. His current consulting locations include Epworth Eastern Hospital in Box Hill and Box Hill Hospital (Eastern Health) in Box Hill.